In today’s ever-evolving landscape of healthcare revenue cycle management (RCM), providers continue to face a critical challenge: claim denial prediction accuracy. As a result, every denied claim not only delays revenue but also increases administrative workload. Moreover, it significantly reduces operational efficiency. Therefore, in order to maintain financial health and streamline processes, it becomes essential to address claim denials proactively.
However, what if you could predict claim denials before they even happen—with up to 80% claim denial prediction accuracy? In fact, that’s precisely the promise of AI-powered denial prediction. As a result, it is rapidly transforming how medical practices manage and optimize their revenue cycles.
🔍 The Cost of Claim Denials in Healthcare
According to the American Medical Association (AMA), denial rates range from 5% to 10% across providers. Consequently, billions are lost annually due to incorrect or incomplete claims. In addition, common causes of denials include the following:
- Eligibility issues
- Incorrect patient demographics
- Coding errors
- Lack of medical necessity documentation
Traditionally, most practices address denials after they occur—reworking and resubmitting claims. But this reactive approach leads to inefficiencies, cash flow delays, and lost time.
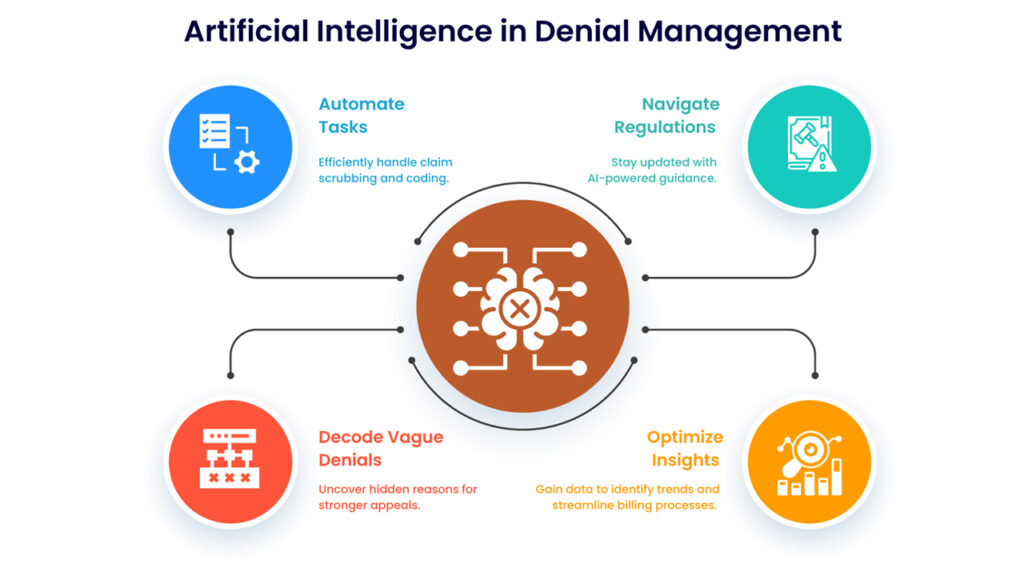
⚙️ The Role of AI in Predicting Claim Denials
Artificial intelligence (AI) has introduced a game-changing paradigm: predictive denial management. By analyzing massive datasets of historical claims and denial reasons, AI models can now identify potential errors in real-time, before a claim is ever submitted.
What Does 80% Accuracy Really Mean?
An AI platform with 80% denial prediction accuracy can correctly flag 8 out of every 10 claims likely to be denied. This level of precision empowers providers to proactively fix issues, reducing rework and increasing clean claim rates—which directly impacts revenue.
One example of such a solution is Clearclaim by aiclaim, a robust AI-driven engine that integrates with your existing RCM workflows and predicts denials with up to 80% accuracy. It supports X12 837 EDI files, offers API integrations, and fits seamlessly into practice management systems.
✅ Benefits of AI-Powered Denial Prediction
1. Increased Clean Claim Rate
AI identifies common pitfalls before submission, reducing the need for appeals or corrections. This directly improves your first-pass resolution rate—a key metric in RCM performance.
2. Improved Cash Flow
With fewer denials, payments are received faster. Clean claims get processed more quickly by payers, leading to accelerated reimbursements.
3. Lower Administrative Costs
Denials require staff time to analyze, fix, and resubmit claims. Predictive AI drastically reduces this labor, freeing your team for more critical tasks.
4. Smarter Insights for Future Submissions
AI doesn’t just flag problems—it learns. Platforms like aiclaim provide denial insights, root cause analysis, and pattern recognition to guide your billing team in improving future performance.
5. Reduced Patient Frustration
Fewer claim delays mean patients aren’t surprised by unexpected bills or long reimbursement times. This leads to better patient experiences and stronger provider-patient relationships.
🔧 How to Integrate AI Denial Prediction into Your RCM Strategy
Adopting AI for claim denial management doesn’t require overhauling your entire billing system. Here’s how to get started:
➤ Evaluate Your Current Denial Rates
Identify where most denials are occurring. Are they coding-related? Eligibility-based? Understanding your baseline is essential for measuring AI impact.
➤ Choose a Compatible AI Partner
Opt for solutions that support X12 837 formats, API access, and easy integration. aiclaim’s Clearclaim engine offers a seamless setup with zero workflow disruptions.
➤ Start Small, Then Scale
Most platforms offer free trials or limited usage (like aiclaim’s 50 free claims). Use this to test prediction accuracy, evaluate results, and gradually roll out across your billing system.
➤ Train Your Staff
Your billing team needs to understand how to interpret AI-predicted denials and fix issues proactively. Use internal dashboards and reports to keep everyone aligned.
📊 Real-World Use Case
A mid-sized multi-specialty clinic used aiclaim’s Clearclaim tool during its alpha phase. Within 30 days:
- Denials dropped by 42%
- Clean claim rate increased from 84% to 92%
- Administrative rework time was cut in half
This translated into faster reimbursements and a 15% increase in net collections—all without changing their existing RCM system.
🛠️ Future-Proofing Your RCM Strategy
With upcoming features like Agentic Denial Workup (AI agents automatically handling denied claims) and real-time denial analytics dashboards, platforms like aiclaim are not only solving today’s problems—they’re preparing providers for tomorrow’s challenges.
🔚 Conclusion
80% prediction accuracy isn’t just a number—it’s a competitive advantage. With AI-powered denial prediction, healthcare organizations can transform their revenue cycle, reduce operational costs, and deliver better patient experiences.
If your practice is ready to reduce denials and improve cash flow, explore how Clearclaim by aiclaim can help. Start with 50 free claims and see the impact for yourself.