Aiclaim helps healthcare providers turn claim denials into successful reimbursements through data-driven and AI-powered Denial Management solutions. Our comprehensive RCM denial management system minimizes revenue leakage, streamlines processes, and enhances your organization’s cash flow with accuracy and efficiency.
Denial Management is a vital component of effective Revenue Cycle Management (RCM) that focuses on identifying, analyzing, and resolving denied or rejected claims. At Aiclaim, we deliver end-to-end Denial Management services that reduce denials, enhance claim accuracy, and ensure faster reimbursements.
Our experts leverage advanced analytics and AI-driven insights to uncover the root causes of claim denials, ensuring that every submission meets payer compliance standards. By implementing proactive denial prevention measures, timely follow-ups, and comprehensive documentation, Aiclaim helps providers recover lost revenue, improve cash flow, and strengthen their financial health through smarter RCM processes.
With Aiclaim’s AI-powered denial management solutions, healthcare organizations can efficiently recover denied claims, optimize billing workflows, and maintain strong payer relationships—resulting in greater financial stability and sustainable revenue growth.
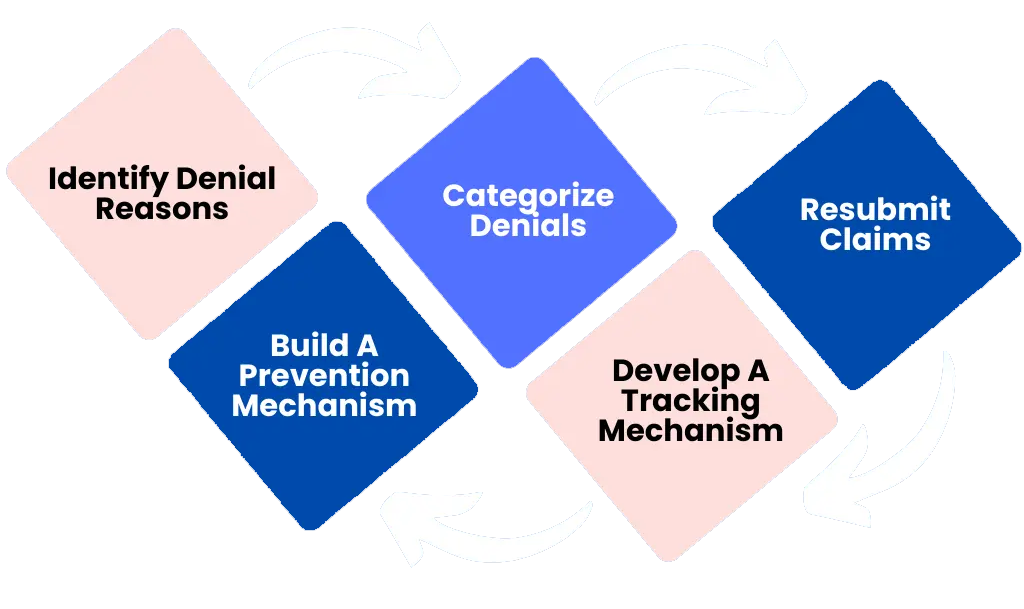
Denial Identification & Categorization: Our experts thoroughly review denied claims to identify key issues, categorize them accurately, and apply data-driven strategies for faster resolution.
Root Cause Analysis : Using AI and analytics, we detect underlying causes such as coding inaccuracies, missing documentation, or eligibility mismatches that lead to denials.
Appeals Management : Our RCM specialists handle appeal preparation and submission with precision, ensuring maximum approval success rates and faster reimbursements.
Prevention Strategies : We collaborate with your billing teams to implement denial prevention plans that reduce recurrence and strengthen claim accuracy.
Comprehensive Reporting : Get real-time reports, denial trends, and actionable insights to monitor performance and make informed financial decisions.
Improved Cash Flow : Maximize revenue by converting denied claims into paid reimbursements efficiently.
Higher Claim Approval Rates : Boost approval ratios through optimized claim submissions and proactive management.
Cost Savings : Eliminate unnecessary rework and appeal costs with accurate first-time submissions.
Compliance Assurance : Ensure compliance with payer regulations and maintain audit-ready documentation.
Aiclaim specializes in resolving common and complex denial causes, preventing future payment delays and lost revenue opportunities.
Expertise : A dedicated team of RCM and Denial Management specialists with years of industry experience.
Technology-Driven : AI-powered analytics and automation tools designed for accuracy, speed, and efficiency.
Customized Solutions : Tailored denial management strategies that adapt to your healthcare organization’s specific needs.
End-to-End Support : From denial prevention to appeals management, Aiclaim provides complete RCM support for better results.
Stop losing revenue to claim denials. Partner with Aiclaim and implement AI-driven Denial Management solutions that ensure faster reimbursements and improved financial outcomes.