In today’s insurance industry, speed, accuracy, and customer satisfaction determine success. However, manual claims management remains one of the biggest bottlenecks in operations. From data entry to verification, each stage consumes time and resources—leading to delays, errors, and revenue leakage. Fortunately, AI claims automation is redefining the landscape by turning manual workflows into intelligent, self-learning systems that process claims faster, smarter, and more accurately than ever before.
What Is AI Claims Automation?
AI claims automation is the use of artificial intelligence (AI), machine learning (ML), computer vision, and natural language processing (NLP) to streamline every stage of the claims process—from submission to settlement. Unlike rule-based systems that rely solely on predefined conditions, AI automation learns from historical data and continuously improves. As a result, it not only automates repetitive tasks but also identifies patterns, detects anomalies, and predicts potential denials before they occur.
In essence, AI claims automation enables insurers and healthcare providers to process claims in real time with minimal manual intervention, improving both speed and accuracy.
Why AI Claims Automation Matters
The traditional claims process is complex and error-prone. But with AI automation, organizations can achieve:
1. Faster Processing and Turnaround Time
AI systems automatically validate data, cross-check documents, and flag inconsistencies within seconds. Therefore, what previously took days now happens in minutes.
2. Improved Accuracy and Reduced Errors
Machine learning models analyze thousands of past claims to learn from mistakes and minimize data entry errors. Consequently, insurers can trust their data and make better decisions.
3. Fraud Detection and Prevention
Through predictive analytics and behavioral modeling, AI identifies suspicious claim patterns before payouts occur. Moreover, continuous monitoring ensures that fraudulent activity is caught early.
4. Cost Efficiency and Scalability
Automating manual work reduces administrative costs, while AI algorithms allow businesses to handle larger claim volumes without additional staffing.
5. Enhanced Customer Experience
Customers benefit from faster approvals, transparent communication, and minimal paperwork—leading to higher satisfaction and loyalty.
How AI Claims Automation Works
AI claims automation integrates multiple technologies to create a seamless workflow:
1. Data Ingestion and Extraction
AI-powered OCR and NLP extract information from documents, PDFs, and scanned forms. Therefore, even unstructured data becomes searchable and usable.
2. Validation and Verification
The system cross-references patient details, policy numbers, and service codes with internal and external databases to verify eligibility and compliance.
3. Predictive Modeling
Machine learning models assess the likelihood of claim approval or denial based on historical data trends. As a result, insurers can proactively correct potential issues before submission.
4. Fraud Detection Algorithms
Advanced AI systems compare current claims with historical fraud cases, flagging anomalies that may require manual review.
5. Automated Decision-Making
AI engines determine the appropriate next step—auto-approve, request more information, or route to a claims adjuster—based on confidence scores.
6. Continuous Learning and Optimization
Over time, AI models learn from outcomes, continuously refining their accuracy and decision-making process.

Benefits for Insurers and Healthcare Providers
For Insurers:
- Reduced claim cycle time and operational cost
- Enhanced fraud prevention capabilities
- Improved compliance and audit readiness
- Greater scalability and transparency
For Healthcare Providers:
- Fewer denials and re-submissions
- Streamlined documentation and coding validation
- Faster reimbursements and improved cash flow
- Better patient satisfaction through quicker resolution
Real-World Impact of AI Claims Automation
Across the insurance and healthcare industries, companies are witnessing measurable outcomes:
- 80% faster claim processing using AI-based validation tools.
- 50% reduction in claim denials due to proactive error detection.
- 35% improvement in fraud identification rates, thanks to predictive analytics.
- Significant cost savings, as fewer manual interventions are required.
Moreover, these systems adapt continuously. Therefore, each processed claim becomes a new learning input, enhancing future accuracy and reliability.
Challenges and How AI Overcomes Them
Data Quality Issues: AI automation depends on clean, structured data. Advanced preprocessing and data cleaning algorithms now ensure higher accuracy.
Legacy System Integration: Many insurers operate on outdated systems. However, modern AI platforms like Aiclaim integrate smoothly via APIs and middleware, enabling seamless automation without full system replacement.
Regulatory Compliance: AI ensures compliance by automatically validating data against local and international insurance regulations, maintaining audit trails for every transaction.
Employee Adoption: By automating repetitive tasks, AI allows human teams to focus on customer service and complex decision-making, improving morale and productivity.
Future of AI Claims Automation
As AI models grow more sophisticated, the future of claims management will become zero-touch—where claims are automatically verified, approved, and settled without human intervention unless exceptions occur. Predictive and generative AI will soon enable personalized claim responses, dynamic risk scoring, and instant settlement based on verified data.
Additionally, emerging technologies such as agentic AI and large language models (LLMs) are expected to enhance context understanding, automate exception handling, and drive complete end-to-end claims management.
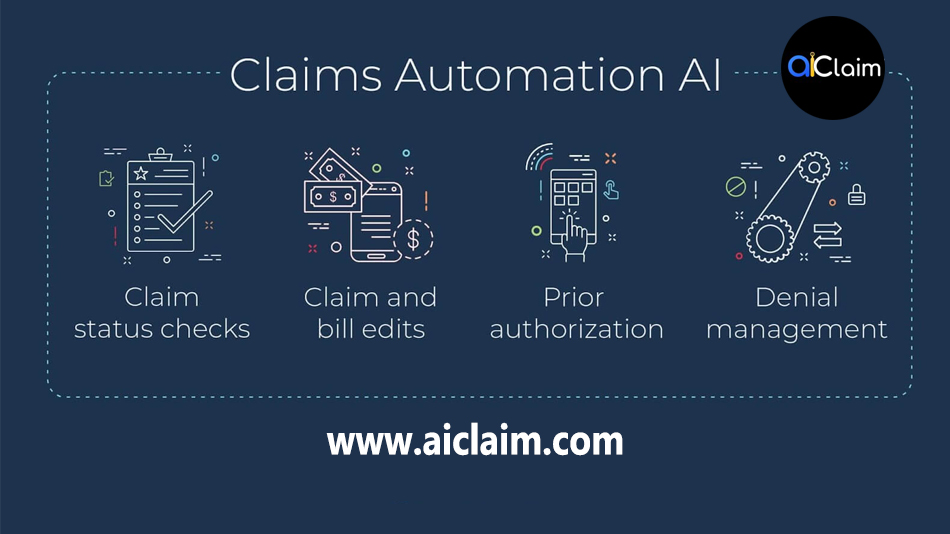
How Aiclaim Leads the Transformation
At Aiclaim.com, we leverage advanced AI models to automate the entire claim lifecycle. Our intelligent platform integrates predictive analytics, document understanding, fraud detection, and real-time reporting to ensure:
- Faster approvals through pre-submission validation
- Fewer denials via AI-powered risk analysis
- Seamless integrations with existing ERP and CRM systems
- Actionable insights through advanced analytics and dashboards
Through continuous innovation and machine learning, Aiclaim is empowering providers and payers to predict, prevent, and profit with next-generation claims automation.
Conclusion
The future of insurance and healthcare claim management is undeniably intelligent. With AI claims automation, organizations can transition from reactive claim handling to proactive optimization—saving time, reducing costs, and improving customer satisfaction.
As competition rises and digital transformation accelerates, adopting AI-driven automation is no longer optional; it’s essential. Therefore, now is the time to embrace automation, optimize workflows, and let AI lead the way toward a smarter, faster, and more efficient claims ecosystem.