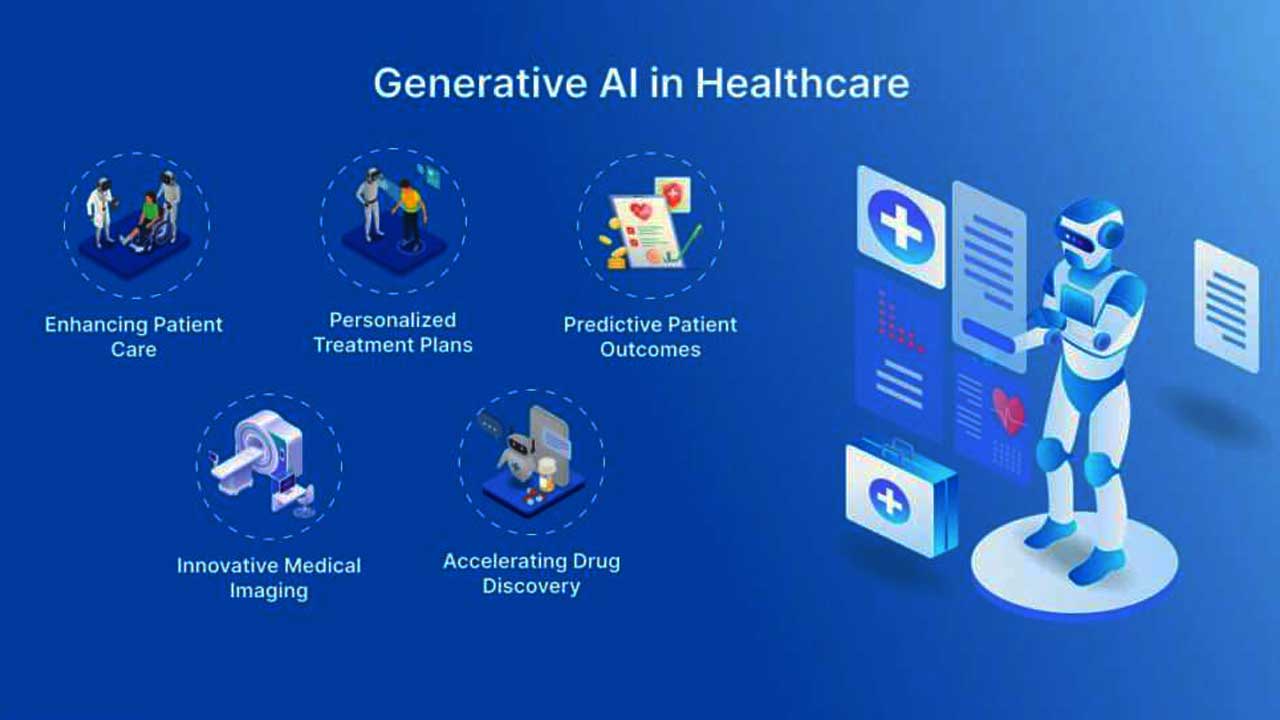
The healthcare industry is undergoing a major transformation, with Artificial Intelligence (AI) taking center stage. Among its many applications, AI-powered tools are revolutionizing healthcare revenue cycles and Revenue Cycle Management (RCM) by enhancing financial efficiency, reducing errors, and improving patient satisfaction. These tools streamline operations, helping healthcare providers achieve better financial outcomes while boosting overall operational effectiveness.
In this blog, we explore the top five AI-powered tools that are enhancing healthcare revenue cycles and transforming how providers manage billing, coding, and payments.
1. Predictive Analytics for Claim Denial Management
Claim denials have been a persistent challenge for healthcare providers, impacting cash flow and increasing administrative workload. AI-powered predictive analytics tools tackle this issue by:
- Analyzing historical claim data to predict potential errors or denials.
- Flagging real-time issues to minimize rejections.
- Providing actionable insights to optimize the claim submission process.
Example Tool: Olive AI
Olive uses machine learning to streamline claim processing, reducing denials and significantly improving approval rates.
2. Robotic Process Automation (RPA) for Billing
Manual billing processes are not only time-consuming but also prone to errors. AI-powered Robotic Process Automation (RPA) tools solve this problem by automating repetitive billing tasks. Key benefits include:
- Automating claims submission and payment posting.
- Eliminating manual errors in data entry.
- Enhancing the efficiency of revenue collection.
Example Tool: Automation Anywhere
This RPA platform automates critical billing processes, ensuring accuracy while saving time and resources.
3. Intelligent Coding Assistants
Accurate medical coding is crucial for proper reimbursements, but it’s often challenging to maintain accuracy due to complex regulations. AI-powered coding tools assist by:
- Automating the selection of appropriate codes based on medical records.
- Reducing human errors that lead to under-coding or over-coding.
- Ensuring compliance with constantly changing coding regulations.
Example Tool: 3M CodeFinder AI
This intelligent coding assistant leverages AI to deliver precise and compliant coding recommendations.
4. Patient Payment Estimation Tools
Transparent billing is essential for building trust with patients. AI-based patient payment estimation tools improve transparency by:
- Generating accurate cost estimates for patients based on their insurance coverage.
- Enhancing patient understanding of financial responsibilities before treatment.
- Increasing the likelihood of upfront payments.
Example Tool: ZOLL AR Boost
This tool provides accurate patient payment estimates, helping patients and providers have clearer financial discussions.
5. AI-Powered Chatbots for Patient Billing Queries
Billing inquiries often overwhelm administrative staff, causing delays and dissatisfaction. AI-powered chatbots alleviate this burden by:
- Offering real-time answers to billing-related questions.
- Suggesting payment plan options for patients.
- Enhancing overall patient satisfaction by ensuring quick and efficient responses.
Example Tool: Ada Health
Ada’s conversational AI platform efficiently addresses billing and payment-related queries, freeing up administrative resources.
Benefits of AI in Healthcare Revenue Cycles
Implementing AI-powered tools in RCM offers several advantages, including:
- Reduced Administrative Burden: Automation allows staff to focus on strategic activities rather than repetitive tasks.
- Improved Financial Outcomes: Accurate billing and coding minimize claim denials and optimize reimbursements.
- Increased Patient Satisfaction: Transparent billing and efficient payment processing improve the patient experience.
- Regulatory Compliance: AI ensures adherence to evolving healthcare regulations and standards.
Conclusion
AI-powered tools are revolutionizing healthcare revenue cycle management, making processes more efficient, accurate, and patient-focused. By investing in these advanced solutions, healthcare providers can improve operational efficiency, enhance financial performance, and deliver better patient experiences. The future of healthcare RCM is AI-driven, and the time to adopt these tools is now.