In today’s rapidly evolving healthcare landscape, hospitals and physician groups are increasingly evaluating the ROI of claims automation. With rising patient volumes and more complex reimbursement models, the pressure to enhance operational efficiency, improve cash flow, and minimize revenue leakage has never been greater. As a result, traditional manual approaches to claims management are proving inadequate, making AI-driven claims automation solutions a strategic necessity.
Consequently, more and more healthcare providers are turning to AI-powered claims automation solutions to address these challenges. But before making such an investment, one critical question arises: What is the true Return on Investment (ROI) of claims automation?
In this blog, we will delve deep into the financial, operational, and strategic ROI of implementing claims automation software, specifically for hospitals and physician groups.

The Current Challenges in Healthcare Claims Management
First and foremost, it’s important to understand the pain points associated with traditional, manual claims processing:
- High rates of claim denials and rejections
- Lengthy claims turnaround times
- Increased administrative overhead
- Poor cash flow management
- Limited real-time visibility into revenue cycle performance
Moreover, manual processes are often error-prone. Even minor mistakes in patient data, coding, or documentation can result in claim rejections, payment delays, or even compliance risks.
As a result, revenue leakage becomes inevitable, and staff burnout increases due to repetitive, low-value tasks.
What is Claims Automation?
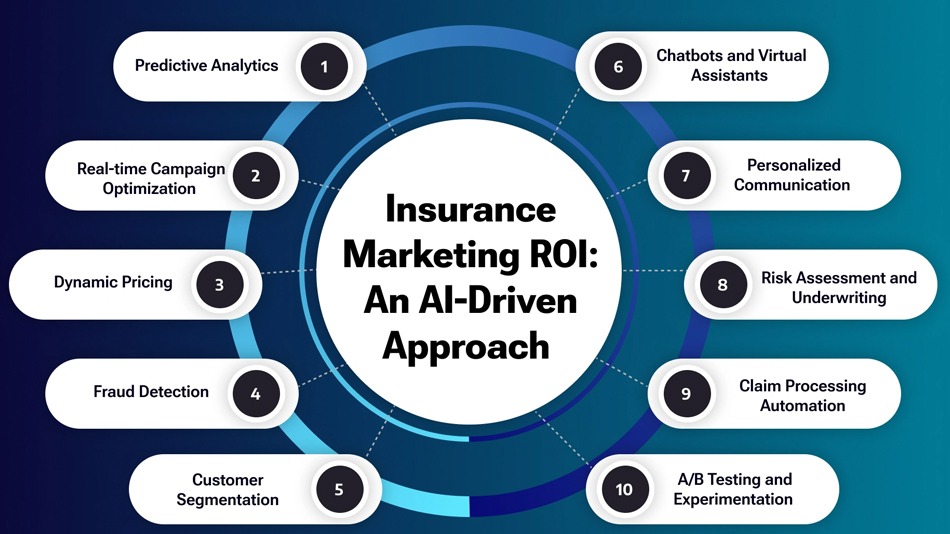
To address these pain points, claims automation leverages Artificial Intelligence (AI) and Machine Learning (ML) technologies to streamline the entire claims lifecycle.
In other words, from patient eligibility verification to claim submission, status tracking, denial management, and payment posting, an AI-driven claims automation platform like Aiclaim handles it all.
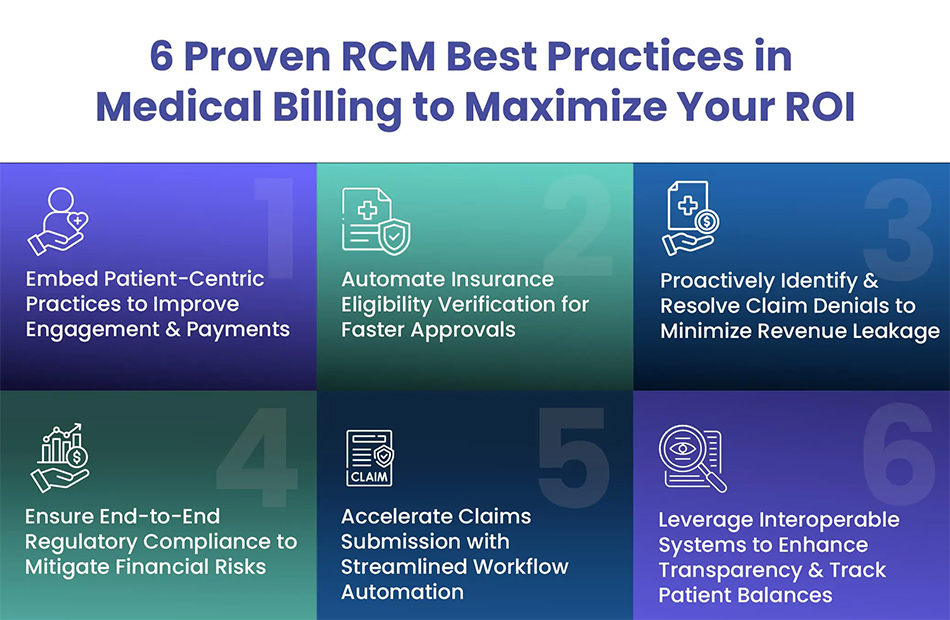
Additionally, these solutions integrate seamlessly with existing Electronic Health Records (EHR) and practice management systems, making the transition smooth and disruption-free.
Key ROI Drivers of Claims Automation for Hospitals and Physician Groups
Let’s explore the various ways in which claims automation delivers measurable ROI:
1. Faster Claims Processing Times
To begin with, one of the most immediate and visible benefits of claims automation is faster claims processing.
Traditionally, it takes days—or even weeks—for claims to move from submission to payment. However, with AI-powered claims management, the entire process can be accelerated by up to 70%.
As a result, cash flow improves, and healthcare providers can better manage their working capital.
For example, what once took 30 days for payment can now take just 10 days, dramatically improving revenue cycle velocity.
2. Reduction in Denial Rates
Moreover, claims automation platforms actively analyze claims data in real-time. By detecting errors before submission, these systems significantly reduce claim denial rates.
Common causes like:
- Incomplete patient information
- Incorrect medical coding
- Authorization issues
- Billing inconsistencies
…are flagged instantly.
Consequently, providers experience a higher first-pass acceptance rate, leading to fewer resubmissions, fewer appeals, and faster payments.
Hospitals using solutions like Aiclaim report up to a 45% reduction in denial rates, making this one of the most compelling ROI factors.
3. Lower Administrative Costs
Furthermore, by automating time-consuming tasks such as data entry, claims status follow-ups, and manual reporting, healthcare organizations can achieve substantial cost savings.
In fact, studies show that administrative costs per claim can drop by as much as 50-60% after implementing claims automation.
To put it differently, fewer staff hours are spent on repetitive tasks, allowing hospitals and physician groups to reallocate resources to higher-value activities like patient care and revenue optimization.
4. Improved Staff Productivity and Satisfaction
Additionally, reducing the administrative burden means that healthcare staff experience less burnout and higher job satisfaction.
As a result, organizations see lower employee turnover rates, saving on recruitment and training costs.
For example, with automation in place, staff can focus more on:
- Patient engagement
- Complex claims resolution
- Revenue cycle strategy
- Data analysis and forecasting
Consequently, overall organizational efficiency improves.
5. Enhanced Data Accuracy and Compliance
It’s equally important to highlight the compliance benefits of AI-driven claims management.
Regulatory compliance in healthcare billing is non-negotiable. However, manual processes increase the risk of coding errors, missing documentation, and HIPAA violations.
By contrast, claims automation tools like Aiclaim ensure that all claims meet payer-specific guidelines.
Furthermore, built-in validation checks and automated audit trails help providers stay compliant, thereby reducing the risk of penalties and audits.
6. Real-Time Analytics and Reporting
Another significant ROI driver is the ability to gain real-time insights into your revenue cycle performance.
With traditional systems, reporting often involves pulling outdated data manually. However, AI-powered claims solutions provide:
- Live dashboards
- Customizable reports
- Predictive analytics
This enables CFOs, revenue cycle managers, and billing teams to identify bottlenecks quickly, track KPIs, and implement corrective actions proactively.
For instance, metrics like denial rates, days in A/R, and average reimbursement timelines are readily available at a glance.
Financial ROI: By the Numbers
Let’s translate these benefits into concrete financial terms:
| Key Metric | Before Automation | After Automation | % Improvement |
|---|---|---|---|
| Average Days to Payment | 30 days | 10 days | 66% Faster |
| Denial Rate | 15% | 5% | 66% Reduction |
| Cost per Claim | $7 | $3 | 57% Savings |
| Staff Hours per Month | 500 hours | 200 hours | 60% Reduction |
| Annual Admin Savings | $0 | $150,000+ | Significant |
Therefore, hospitals and physician groups can realistically expect to recoup their investment in claims automation within the first year, depending on scale and claim volume.
A Real-World Example: Aiclaim Success Story
To further illustrate, consider a mid-sized hospital that partnered with Aiclaim for its RCM automation needs.
Before implementation:
❌ High denial rates
❌ Slow payment cycles
❌ Overburdened billing staff
After 6 months of automation:
✅ 45% reduction in denials
✅ 60% faster reimbursement turnaround
✅ $150,000+ in annual cost savings
✅ Improved staff morale and productivity
Clearly, the ROI was both financial and operational, validating the decision to adopt AI-powered claims automation.
Strategic ROI: Looking Beyond Short-Term Gains
While the financial benefits are undeniable, the long-term strategic value of claims automation is equally important.
For instance:
- Future-proofing your revenue cycle operations
- Enhancing patient experience with faster billing
- Reducing dependency on manual labor
- Staying compliant with ever-changing payer regulations
- Gaining a competitive edge in the healthcare market
Moreover, as healthcare reimbursement models continue to evolve, having an automated system in place ensures that your organization can adapt quickly and remain profitable.
Conclusion: Is Claims Automation Worth the Investment?
In conclusion, the ROI of claims automation for hospitals and physician groups extends far beyond simple cost savings.
It offers:
✅ Financial improvements (cost reduction, faster payments)
✅ Operational efficiency (reduced denials, lower A/R days)
✅ Staff productivity (focus on higher-value tasks)
✅ Compliance and accuracy (minimized regulatory risk)
✅ Strategic readiness (scalable and future-proof systems)
Given the high stakes in today’s healthcare environment, investing in a robust claims automation solution like Aiclaim is no longer a luxury—it’s a necessity for sustainable growth.
✅ Ready to Maximize Your ROI with Aiclaim?
If you’re ready to transform your claims process and experience real, measurable ROI, contact Aiclaim today.
📱 Phone: +1 (630) 686-8684
📧 Email: info@aiclaim.com
🌐 Website: www.aiclaim.com
Let’s help you unlock the full potential of AI-powered healthcare claims automation