Introduction
In today’s ever-evolving healthcare landscape, financial stability is a top priority for providers. However, many healthcare organizations face revenue leakage, which directly impacts profitability and sustainability. This is where Revenue Integrity in Healthcare comes into play. Ensuring compliance, accurate billing, and efficient reimbursement processes can prevent revenue loss and optimize financial performance.
In this blog, we will explore what revenue integrity in healthcare means, why it is crucial, common causes of revenue leakage, and effective strategies to maximize reimbursement.

What is Revenue Integrity in Healthcare?
Revenue Integrity in Healthcare refers to the process of ensuring that revenue is accurately captured, billed, and collected while maintaining compliance with industry regulations. It bridges the gap between clinical operations, coding, billing, and reimbursement, ensuring that every service provided is correctly documented and paid for appropriately.
When done effectively, revenue integrity helps healthcare providers:
- Prevent financial losses due to inaccurate billing or coding errors
- Improve compliance with government and payer regulations
- Streamline reimbursement processes to maintain cash flow stability
- Enhance overall patient experience by minimizing billing discrepancies
Why is Revenue Integrity Important?
Many healthcare providers face unnoticed revenue leaks that can lead to significant financial losses over time. Without a structured revenue integrity program, organizations risk non-compliance penalties, claim denials, and operational inefficiencies.
According to industry reports, billing errors account for billions in lost revenue every year, making revenue integrity a crucial aspect of financial health. Additionally, regulatory bodies such as CMS (Centers for Medicare & Medicaid Services) and HIPAA (Health Insurance Portability and Accountability Act) mandate strict compliance to avoid fraudulent claims and penalties.
Common Causes of Revenue Leakage
Understanding the root causes of revenue leakage is essential for implementing an effective revenue integrity strategy. Here are some common factors:
1. Inaccurate Medical Coding
Incorrect or incomplete medical coding can result in claim denials or underpayments. CPT, ICD-10, and HCPCS codes must be accurately documented to reflect the provided services. Investing in regular coding audits and training can reduce errors.
2. Billing Errors
Duplicate billing, incorrect patient information, and missing charges can lead to denied claims. Implementing automated billing systems can significantly reduce manual errors and streamline claim processing.
3. Lack of Compliance with Regulatory Standards
Failure to adhere to Medicare, Medicaid, and private payer requirements can result in denied or delayed reimbursements. Keeping up with regulatory changes is vital to ensure compliance.
4. Underpayment and Denied Claims
Payers may deny claims due to missing documentation or non-compliance with coding guidelines. A strong denial management strategy is necessary to appeal rejected claims and recover lost revenue.
5. Failure to Capture All Billable Services
Often, providers miss billing for additional services such as telemedicine consultations, follow-ups, or procedures that were performed but not documented properly.

Strategies to Prevent Revenue Leakage and Maximize Reimbursement
Now that we understand the causes of revenue leakage, let’s explore strategies to enhance revenue integrity in healthcare.
1. Implement Automated Revenue Cycle Management (RCM) Systems
Using AI-driven revenue cycle management (RCM) software can help reduce errors, automate coding, and improve claim tracking. Automated systems ensure accurate charge capture, reducing the risk of missed revenue opportunities.
2. Conduct Regular Audits and Compliance Checks
Internal and external audits help identify potential issues before they escalate. Regular compliance checks ensure that billing and coding processes align with industry standards.
- Internal audits can detect recurring coding errors.
- External audits, conducted by third-party experts, provide an unbiased assessment of revenue integrity.
3. Enhance Staff Training and Education
Keeping billing and coding staff up to date with current regulations and industry best practices is crucial. Regular training sessions help reduce coding errors and improve claim accuracy.
4. Optimize Denial Management and Appeals Process
Develop a structured denial management process to track and analyze rejected claims. Implementing a strong appeals process ensures that revenue is not lost due to unnecessary denials.
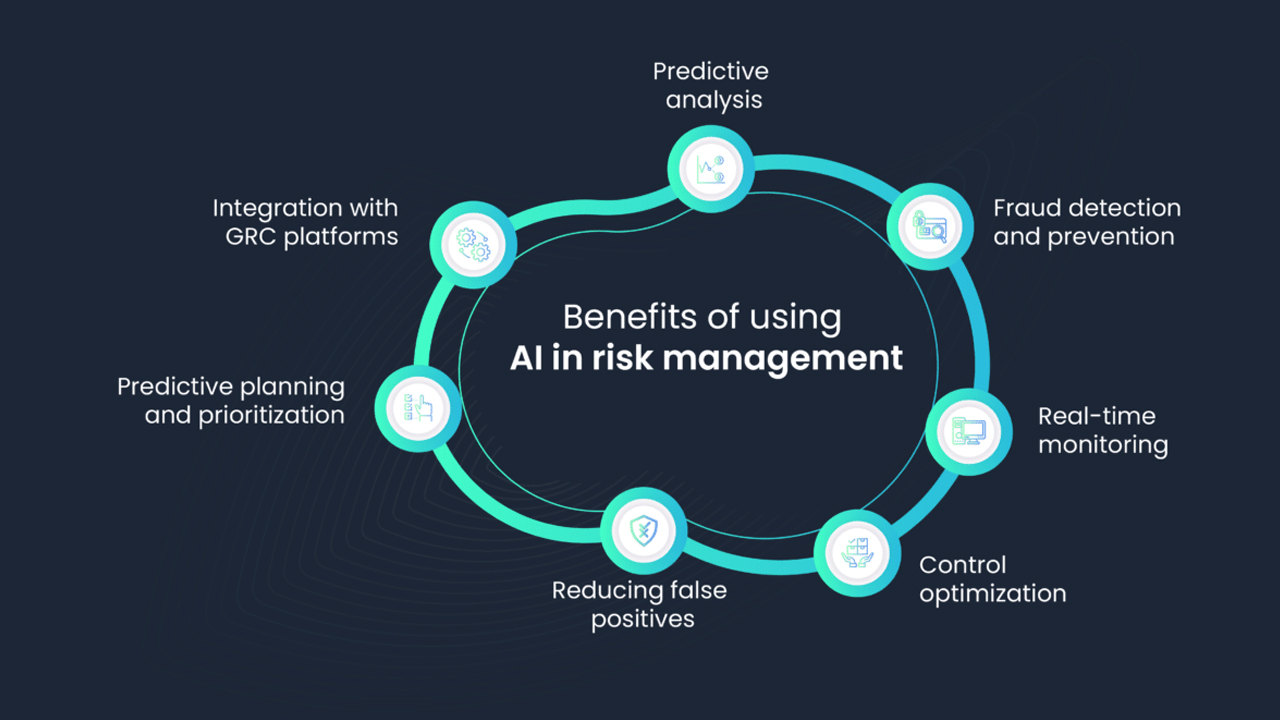
5. Leverage Data Analytics for Revenue Optimization
Using advanced analytics and business intelligence tools helps identify patterns of revenue leakage and optimize reimbursement. Predictive analytics can help healthcare providers proactively address revenue gaps.
6. Ensure Transparent Patient Billing and Payment Processes
Clear and transparent patient billing reduces disputes and improves patient satisfaction. Offering flexible payment options and digital billing solutions enhances the patient experience while ensuring timely payments.
Conclusion
In today’s complex healthcare environment, ensuring Revenue Integrity in Healthcare is not just a financial necessity but also a compliance requirement. By implementing best practices such as automated revenue cycle management, regular audits, staff training, and effective denial management, healthcare providers can significantly reduce revenue leakage and maximize reimbursements.
At Aiclaim, we specialize in providing cutting-edge solutions to enhance revenue integrity and optimize financial performance for healthcare providers. If you are looking to improve your revenue cycle and reduce financial risks, contact us today!
Related Resources:
- Understanding Revenue Cycle Management (RCM)
- Common Medical Billing Mistakes and How to Avoid Them
- External Resource: CMS Regulations on Medical Billing
Ready to strengthen your revenue integrity strategy? Visit Aiclaim to explore our healthcare revenue solutions today!