The healthcare industry is entering a new era—one where claim denials are no longer accepted as a standard operational burden. As we step into 2026, healthcare providers are prioritizing AI-powered denial management solutions to reduce administrative complexity, accelerate reimbursements, and improve financial outcomes. With rising payer scrutiny and increasing regulatory changes, traditional denial management workflows are no longer sustainable.
Today, the question is no longer “Can AI reduce denials?”
Instead, it is now becoming clear that the real question is:
👉 “How close can we get to zero denials using AI?”
As a result, healthcare providers are no longer waiting for claims to fail before taking action. At Aiclaim, the future of denial management is already unfolding. Furthermore, with advanced automation, predictive analytics, and machine learning, healthcare organizations can finally prevent denials before they occur. Consequently, this shift allows providers to optimize revenue cycle operations faster, smarter, and more efficiently than ever before.
🌟 The Growing Challenge: Why Claim Denials Are Still Increasing in 2025
Although technology has improved across the healthcare ecosystem, claim denials continue to rise each year. In fact, denial trends reveal a concerning revenue gap. Recent studies indicate that:
- Over 18–22% of claims still face denial on the first submission.
- Nearly 65% of denied claims are never resubmitted or appealed.
- Therefore, providers lose millions annually due to avoidable coding, documentation, and authorization issues.
Additionally, compliance demands are increasing while payer rules are becoming more complex and inconsistent. Meanwhile, staffing shortages and manual workflows create bottlenecks that slow down the reimbursement timeline.
As value-based care expands and regulatory reporting intensifies, manual denial management processes are no longer sustainable. Thus, healthcare organizations must adopt intelligent solutions that eliminate repetitive errors, enhance compliance, and maximize reimbursement potential.
🚀 Why 2026 Marks the Turning Point
Due to accelerating financial pressure, shrinking margins, and evolving payer requirements, providers are finally prioritizing automation. Therefore, 2026 is becoming the year when AI transforms denial management from a reactive fix into a proactive prevention strategy.
Ultimately, AI is not just improving workflows—it is rewriting the entire denial management model.

🚀 AI-Powered Denial Management: A Game-Changing Shift in RCM
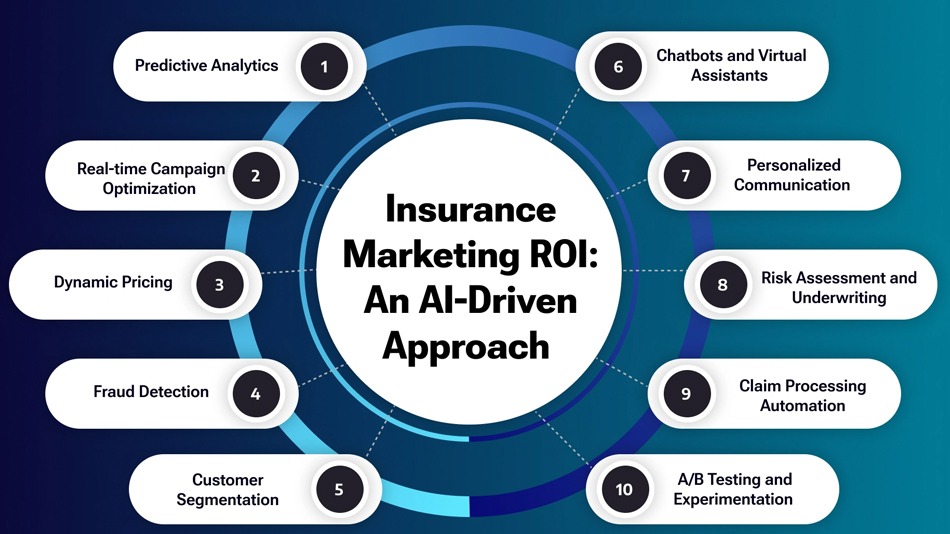
AI is not simply automating tasks — it is transforming how errors are predicted, prevented, and resolved. Instead of waiting for denials, healthcare organizations can now use AI-based systems to:
- Identify potential denial triggers
- Automatically validate claim accuracy
- Ensure coding and billing compliance
- Predict denial likelihood in real time
- Generate automatic appeals with payer-specific intelligence
This shift ensures higher first-pass claim acceptance and significantly reduces operational costs.
🧠 How AI Predicts and Prevents Claim Denials Before Submission
AI-powered denial management works by analyzing vast datasets—including payer history, coding patterns, documentation gaps, and regulatory updates.
At Aiclaim, this process includes:
| AI Feature | Benefit |
|---|---|
| Predictive Analytics | Forecast denial probability before submission |
| Automated Coding Validation | Eliminates human-driven documentation and coding errors |
| Payer-Specific Rule Engine | Prevents denials based on changing payer policies |
| Auto-Appeal Generator | Creates compliant, audit-ready appeal letters |
| Real-Time Alerts | Notifies staff before risky claims are submitted |
This approach ensures healthcare providers aren’t just fixing denials—they’re preventing them entirely.
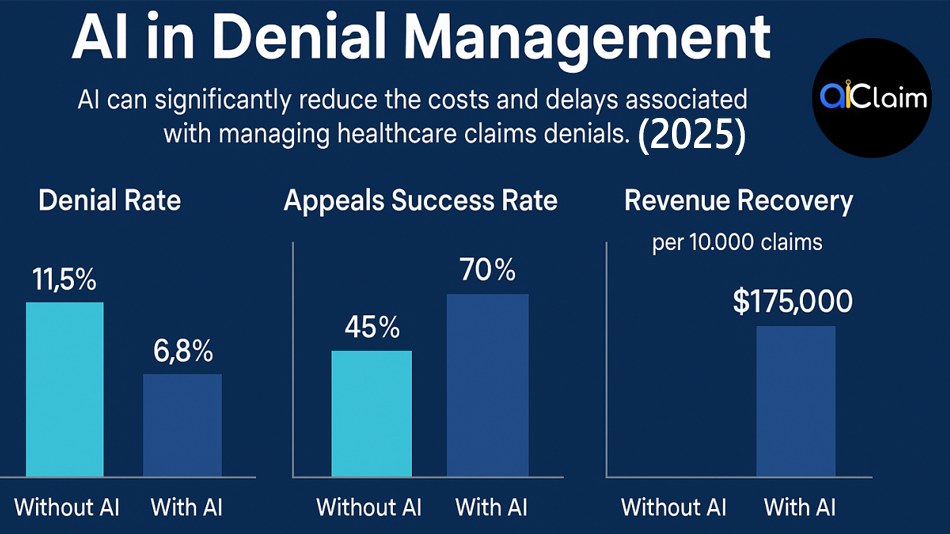
📈 The Financial Impact: Why Zero Denials Is No Longer Impossible
Healthcare organizations adopting AI for denial management see:
- ⬆ 45% to 70% reduction in denials
- ⬆ 25% improvement in first-pass resolution
- ⬆ 35–50% faster reimbursement cycle
- 🕒 70% reduction in administrative workload
- 💰 Recovering millions in lost revenue
In 2026, these results will become the new benchmark.
🔍 Top Reasons Healthcare Providers Choose AI-Powered Denial Management
✔ 1. Reduced Manual Workload and Administrative Stress
AI eliminates repetitive tasks, reducing burnout and improving operational focus.
✔ 2. Improved Compliance and Accuracy
Regulatory updates, payer rules, and coding requirements change frequently — AI keeps your workflow compliant.
✔ 3. Increased Revenue and Cash Flow
With fewer denials, cash flow accelerates, strengthening financial stability.
✔ 4. Transparent Insights and Actionable Reporting
AI-driven dashboards help leaders make data-backed RCM decisions.
🏥 Why Aiclaim Is Leading the AI Denial Management Revolution
Aiclaim offers a comprehensive denial prevention and resolution system built for:
- Hospitals
- Physician groups
- Diagnostic centers
- Healthcare billing companies
- Specialty care providers
Our platform provides:
- 🔹 AI-driven error detection
- 🔹 Instant payer compliance validation
- 🔹 Automated appeals
- 🔹 Real-time denial analytics
- 🔹 Smart RCM workflows designed for zero denial targets
👉 This ensures every claim is accurate, compliant, and optimized before submission.
🔮 Future Outlook: Denial-Free RCM Is Not a Dream—It’s a Roadmap
By 2026 and beyond, healthcare RCM will shift to fully automated denial prevention, where:
- Claims are validated in real time
- Coding is AI-generated and error-free
- Payer requirements are automated
- Denials are predicted before they happen
Organizations embracing AI today will become tomorrow’s financial leaders.
🎯 Conclusion: 2026 — The Year Zero Denials Becomes Reality
The healthcare industry is rapidly advancing, and AI-powered denial management is no longer optional—it’s essential. As automation, predictive intelligence, and compliance engines evolve, the vision of zero claim denials is not just achievable — it’s becoming the new standard.
With Aiclaim, healthcare providers can:
✔ Prevent denials
✔ Improve first-pass resolution rate
✔ Reduce operational costs
✔ Accelerate reimbursements
✔ Unlock lost revenue
👉 Ready to eliminate denials and transform your RCM?
📩 Schedule a personalized demo with Aiclaim today.
🔗 https://www.aiclaim.com/appointment.php