The healthcare revenue cycle management (RCM) market is undergoing a significant transformation, driven by technological advancements and the increasing need for efficient financial processes. Artificial intelligence (AI) is emerging as a key player in this evolution, with the potential to address many pain points faced by healthcare RCM companies. This report explores the current trends in the RCM software world, identifies core challenges faced by healthcare RCM companies, and examines how agentic AI can be leveraged to solve these problems.
Trends in Healthcare RCM Software
The healthcare RCM software market is experiencing robust growth, fueled by several factors:
- Key Trends in Healthcare RCM Software
- Growing Concern Over Revenue Leakage
Healthcare providers are increasingly focusing on reducing revenue leakage caused by inefficient processes, claim denials, and billing inaccuracies. As a solution, RCM software helps identify these issues, optimize revenue capture, and enhance financial performance. - Shift Toward Value-Based Reimbursement Models
With the transition to value-based care, healthcare providers must track quality metrics and patient outcomes to secure reimbursements. Consequently, RCM software plays a vital role in facilitating accurate reporting, ensuring compliance, and demonstrating value in patient care. - Accelerated Adoption of Advanced Software Systems
To streamline workflows and improve data management, healthcare organizations are actively implementing sophisticated software solutions. In this context, RCM software enhances efficiency, reduces administrative burdens, and supports seamless operations. - Rapid Technological Advancements
The RCM software market is evolving quickly, driven by innovations such as AI, automation, and cloud computing. As a result, these advancements improve accuracy, speed up claim processing, and provide better financial insights for healthcare providers. These technologies are enhancing the capabilities of RCM systems, enabling providers to automate tasks, improve accuracy, and reduce costs.
Increasing adoption of AI in RCM is driven by the need to improve efficiency, reduce costs, and address staffing shortages.
Approximately 80% of healthcare executives are ramping up IT and software investments, driven by the rise of AI technologies, including generative AI. These advanced tools enhance efficiency, streamline workflows, and reduce errors across various healthcare operations. In revenue cycle management (RCM), AI-powered solutions play a crucial role in patient registration, eligibility verification, claims processing, denials management, and payment posting. Additionally, generative AI and Large Language Models (LLMs) are gaining momentum in healthcare RCM, enabling automation of complex tasks such as medical coding and claim processing with improved accuracy and efficiency.
Key players in the RCM software market include
| Rank | Vendor | #of Installs | %Market Share |
| 1 | Epic Systems Corporation | 3,465 | 43.91% |
| 2 | Oracle Cerner | 2,241 | 28.40% |
| 3 | MEDITECH | 1,574 | 19.95% |
| 4 | SSI Group | 1,578 | 14.67% |
| 5 | Experian Health | 810 | 10.26% |
Future trends in RCM include:
- Investment in managed RCM services
- Addressing staff shortages and reimbursement model changes
- Improving workflow inefficiencies
- Technological advancements in RCM
- Technology integration
- Reducing medical billing errors
- Patient-centric approaches
- Financial clearance and diverse payment options
- Financial engagement and omnichannel platforms
- Addressing challenges specific to each revenue cycle segment
- Customizable RCM solutions
- The role of strategic partnerships
Current State of Healthcare RCM Software
The current state of healthcare RCM software is characterized by a shift from paper-based to digital systems. Two decades ago, medical billing was primarily paper-based and traditional. Today’s RCM technology features powerful tools that streamline the entire revenue cycle, from patient registration to payment collection. As healthcare operations continue to evolve, RCM has become an essential component, enabling providers to optimize revenue while simultaneously reducing administrative costs. By streamlining billing, claims processing, and payment workflows, RCM not only improves financial performance but also enhances overall efficiency. Consequently, healthcare organizations can allocate more resources toward patient care, ultimately improving both operational and clinical outcomes.
Modern RCM software provides advanced analytics and real-time financial insights, enabling providers to monitor cash flow and identify bottlenecks. HIPAA-compliant RCM technologies help providers meet regulatory requirements, including HIPAA and Meaningful Use, and ensure they are reimbursed accurately and promptly. Many healthcare organizations are now looking at outsourced RCM services to support their billing process.
The healthcare industry is rapidly moving towards digitalization, creating demand for advanced revenue cycle management (RCM) solutions. The increasing number of data silos and unorganized workflows in healthcare settings is leading to market development and growth. Many health systems and hospitals are increasingly investing in advanced technologies to enhance the revenue cycle, including AI, robotic process automation, and automated coding. As a result, these innovations help streamline operations, reduce errors, and improve financial outcomes. In fact, most survey respondents anticipate a significant increase in the total RCM budget allocated to technology solutions, further highlighting the growing reliance on automation and AI-driven tools.
Moreover, the global healthcare revenue cycle management software market continues to expand at a rapid pace. In 2024, the market size was valued at USD 76.91 billion, and it is projected to reach USD 151.01 billion by 2032. With a compound annual growth rate (CAGR) of 8.8% during the forecast period, this substantial growth underscores the increasing demand for efficient and technology-driven RCM solutions across the healthcare industry.
Projected growth of the US revenue cycle management market:
| Source | Market Size in 2024 | Projected Market Size | CAGR | Forecast Period |
| Precedence Research | USD 58.53 billion | USD 175.23 billion | 12% | 2024 to 2034 |

Challenges & Pain Points Faced by Healthcare RCM CompaniesOngoing Challenges in RCM and the Role of Agentic AI
Despite the rapid advancements in RCM software, healthcare organizations continue to face significant challenges. However, with the integration of agentic AI, many of these obstacles can be addressed more effectively.Overcoming Key Challenges in RCM with Agentic AI
Despite advancements in revenue cycle management (RCM), healthcare organizations continue to face several persistent challenges. However, with the integration of agentic AI, these obstacles can be effectively mitigated, leading to improved efficiency, compliance, and financial stability.
Persistent Staffing Shortages
Hiring and retaining skilled revenue cycle management professionals remains a major hurdle for many healthcare organizations. As a result, the increasing reliance on agentic AI is proving to be a valuable solution by automating key tasks such as eligibility verification and prior authorization. Consequently, this not only reduces the workload on human staff but also enhances operational efficiency and minimizes administrative burdens. In the long run, AI-powered automation allows healthcare teams to focus on more complex, high-value tasks.
High Volume of Claim Denials
Claim denials continue to be a significant pain point, as they disrupt cash flow and require substantial time and resources to resolve. Fortunately, agentic AI can address this issue by improving coding and billing accuracy, identifying potential errors before submission, and automating the appeals process. As a result, organizations experience fewer denials, faster reimbursements, and improved financial performance. Additionally, AI-driven predictive analytics help proactively detect patterns that may lead to denials, allowing providers to take corrective action in advance.
Evolving Compliance and Regulatory Requirements
Keeping up with ever-changing billing, coding, and privacy regulations presents an ongoing challenge for healthcare organizations. To address this, agentic AI automates compliance monitoring, ensuring adherence to guidelines while providing real-time updates on regulatory changes. Consequently, organizations can avoid costly penalties and maintain regulatory compliance more efficiently. Moreover, AI-powered tools can flag potential compliance risks before they become major issues, helping providers stay ahead of evolving legal requirements.
Complex Data Management Issues
Managing duplicate medical records, inaccurate patient data, and interoperability challenges often results in errors and inefficiencies. However, agentic AI significantly enhances data management by integrating with various systems, identifying and correcting inconsistencies, and providing a unified view of patient information. As a result, organizations can improve data accuracy, streamline workflows, and enhance overall operational efficiency. Furthermore, AI-driven data validation ensures that critical patient and financial information remains consistent across multiple platforms.
Challenges in the Patient Financial Experience
With rising healthcare costs and ongoing economic uncertainty, many patients struggle to pay their medical bills on time. To address this issue, agentic AI enhances the patient financial experience by offering clear cost breakdowns, flexible payment options, and automated payment reminders. Consequently, healthcare providers can maintain a steady cash flow while also improving patient satisfaction and trust. Additionally, AI-driven chatbots and virtual assistants can provide real-time financial assistance, helping patients better understand their billing options and payment plans.
Frequent Billing and Collection Errors
Errors in billing and collections can result in significant revenue loss while also damaging patient trust. Fortunately, agentic AI helps prevent such errors by automating billing tasks, improving accuracy, and providing real-time feedback to staff. As a result, organizations can reduce financial losses, enhance billing transparency, and improve overall revenue cycle efficiency. Additionally, AI-powered systems can detect anomalies in billing data, allowing for proactive error correction before claims are submitted.
Reliance on Outdated Technology
Many healthcare organizations continue to operate with outdated RCM technology, which hinders efficiency and increases the likelihood of errors. By adopting agentic AI-driven solutions, providers can modernize their systems, improve operational efficiency, and reduce administrative burdens. Furthermore, AI-powered cloud-based RCM solutions enable seamless integration with electronic health records (EHRs) and other essential systems, ensuring a more streamlined and connected revenue cycle.
Lack of Adequate Training and Resources
Insufficient training and limited resources often contribute to inefficiencies in RCM processes. However, agentic AI can bridge this gap by offering real-time guidance and support to staff. Consequently, this reduces the need for extensive training while simultaneously ensuring accuracy and compliance in daily operations. Moreover, AI-driven training modules can personalize learning experiences based on individual employee needs, making professional development more efficient and targeted.
Economic Uncertainty and Financial Pressures
Economic downturns and rising operational costs create financial pressures for healthcare providers, making it essential to optimize revenue capture. In response, agentic AI helps organizations reduce costs, enhance revenue cycle efficiency, and maintain financial stability despite economic challenges. Additionally, AI-driven financial analytics can provide actionable insights, helping organizations make data-driven decisions to navigate economic uncertainty effectively.
Difficulties in Monitoring Claims Processes
Due to the complexity of the RCM process, errors—ranging from inaccurate patient data entry to incorrect ICD-10 code translation—often go unresolved. To overcome this, agentic AI closely monitors and audits every step, verifies ambiguous data with patients, and conducts thorough follow-ups on claims using advanced EHR tools. As a result, organizations can minimize claim errors, reduce rework, and ensure smoother processing. Furthermore, AI-driven real-time alerts help flag potential claim issues before submission, reducing delays and improving reimbursement timelines.
Conclusion
By addressing these challenges with agentic AI, healthcare organizations can significantly improve their RCM processes, enhance efficiency, and maintain compliance. Furthermore, AI-powered automation not only reduces administrative burdens but also improves the overall financial experience for both providers and patients. As the healthcare industry continues to evolve, integrating AI-driven solutions will be key to achieving long-term success and sustainability in revenue cycle management.
Top 5 challenges facing RCM teams in 2024:
- Timely patient collections (48%)
- Managing denials (36%)
- Hiring and training staff (32%)
- Data analytics and reporting (26%)
- Maintaining security and compliance (13%)
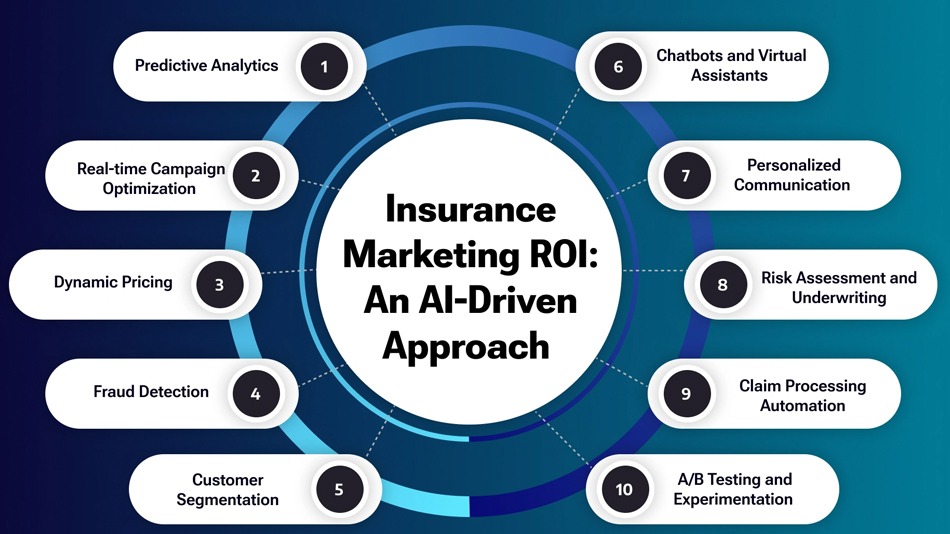
AI in Other Industries
Agentic AI is being used in various industries to solve similar problems:
- Supply Chain Management: Agentic AI is used to optimize supply chains, manage inventory, and predict demand fluctuations. For example, AI agents can continuously monitor the qualifications and capabilities of employees and new hires by analyzing emails, chats, support tickets, and presentations. As a result, they can dynamically adjust training requirements by assigning relevant courses or connecting employees with subject matter experts (SMEs) and mentors. Furthermore, companies are increasingly leveraging AI agents to automate inventory monitoring, ensuring real-time tracking and reducing the risk of stock shortages or overages. Consequently, these advancements help organizations enhance workforce development and streamline operational efficiency.
By automatically placing orders, predicting supply chain disruptions based on external events, and adjusting production schedules, they can maintain optimum inventory levels. - Cybersecurity: AI agents can autonomously monitor network traffic, detect anomalies, and respond to cyber threats in real-time.
- Content Creation: Agentic AI can automate the creation of high-quality, personalized marketing content.
- Software Engineering: AI agents can automate repetitive coding tasks, improving developer productivity.
- Autonomous Transportation: Agentic AI plays a crucial role in self-driving cars and delivery robots.
Agentic AI can be designed to search the web, called application programming interfaces (APIs), or query databases. Agents can fetch real-time information, retrieve updates, or pull specific data points that are critical for decision-making. Agents can initiate and manage tasks such as data logging, real-time monitoring, and trend analysis. They can proactively track and collect data streams from IoT devices, social media feeds, or other systems, providing LLMs with fresh inputs for more informed decision-making and contextual responses.
Potential Benefits of Agentic AI in Healthcare RCM
Agentic AI offers several potential benefits for healthcare RCM:
- Improved Efficiency: AI agents can automate tasks, streamline workflows, and reduce manual errors, leading to significant improvements in efficiency.
- Reduced Costs: By automating tasks and minimizing errors, agentic AI can help reduce operational costs associated with RCM.
- Increased Accuracy: AI agents can improve accuracy in areas like eligibility verification, coding, and claims processing, leading to fewer denials and faster reimbursements.
- Enhanced Compliance: AI agents can help ensure compliance with regulations by automating tasks and monitoring processes for adherence to guidelines.
- Improved Patient Experience: By streamlining processes and reducing errors, agentic AI can contribute to a better patient financial experience.
- Scalability: AI agents can easily scale to handle increasing workloads, making them a valuable asset for growing healthcare organizations.
Agentic AI offers a more comprehensive and integrated approach to RCM automation compared to traditional AI tools.
AI agents work together to create an efficient, error-free RCM process. For example, eligibility verification lays the groundwork for correct prior authorizations, which in turn affects coding, claims submission, and payment posting. When one step falters, inefficiencies multiply—leading to denied claims, delayed reimbursements, and increased administrative costs. AI Agents such as Eligibility Verification Agent (EVA), Claims Automation Agent (CAM), and Payments Posting Agent (PHIL) are the backbone of this transformation. These AI Agents streamline RCM processes, ensuring efficiency and accuracy, allowing healthcare providers to focus on what truly matters: patient care.
AI implementation can improve claim accuracy from the start, helping teams bring in faster, fuller payments.
Every health executive surveyed agreed that AI can bring value to healthcare revenue cycle management. AI in RCM yields positive ROI. Study respondents agree, with 75% saying that AI enhances staff productivity.
Potential Risks of Agentic AI in Healthcare RCM
While agentic AI offers significant potential, it’s essential to consider the risks:
- Data Privacy and Security: Protecting sensitive patient data is crucial when implementing AI in healthcare RCM. Robust cybersecurity measures and compliance with regulations like HIPAA are essential.
- Bias and Fairness: AI algorithms can perpetuate existing biases if not carefully designed and monitored. Ensuring fairness and equity in AI-driven RCM processes is critical.
- Lack of Transparency: Some AI algorithms can be complex and difficult to understand, making it challenging to identify and address errors or biases.
- Over-reliance on AI: It’s important to maintain human oversight and not solely rely on AI for critical decision-making in healthcare RCM.
- Rising Administrative Costs: Handling insurance claims, billing, and payment processing is labor-intensive. With the unique requirements of each payer, managing the paperwork becomes time-consuming and expensive. Administrative costs can quickly spiral out of control, reducing operational efficiency.
- Delayed Reimbursements: Delayed reimbursements are one of the biggest headaches for healthcare providers. Errors in coding, missing information, or claim rejections can put payments on hold, creating cash flow issues that disrupt daily operations and financial planning.
- The Compliance Labyrinth: The healthcare industry is subject to a complex web of regulations and compliance requirements. Navigating this labyrinth can be challenging, especially with the constant changes and updates to rules and guidelines.
Ensuring Compliance and Regulatory Adherence for Agentic AI in Healthcare RCM
Implementing agentic AI in healthcare RCM requires careful consideration of regulatory and compliance requirements:
- HIPAA Compliance: AI systems must comply with HIPAA regulations to protect patient data privacy and security.
- FDA Regulations: The FDA is actively developing guidance on the use of AI in healthcare, including RCM.
- This consideration of accuracy and patient outcomes continues in the scrutiny of AI-enabled systems that have deficits in explainability but produce empirically validated benefits.
- Data Security: Healthcare organizations must implement robust data security measures to protect against breaches and ensure compliance.
- Transparency and Explainability: AI systems should be transparent and explainable to ensure accountability and build trust.
Regulatory compliance is a crucial consideration for implementing agentic AI in healthcare RCM, with HIPAA and FDA guidelines playing a key role.
Artificial intelligence (AI) refers to the development of computer systems capable of performing tasks that typically require human intelligence. This includes tasks such as learning from data, understanding natural language, and making decisions. In the context of healthcare revenue cycle management (RCM), AI is increasingly being used to automate and improve various processes. By applying machine learning, natural language processing, and robotic process automation (RPA), AI helps manage and optimize tasks like coding, billing, and patient interactions. This integration leads to greater accuracy, faster processing times, and overall improvements in financial and operational efficiency within healthcare organizations.
AI technologies are bringing significant improvements to revenue cycle management:
- Improved Coding and Billing Accuracy: AI tools automate the process of coding medical procedures, cutting down on…source them proactively, leading to fewer denials and faster payments.
Agentic AI and Large Language Models (LLMs) are both forms of artificial intelligence, but they serve different purposes and operate in distinct ways. 36
- Agentic AI: Agentic AI is designed to operate autonomously to achieve specific goals. It can make decisions, take…source understanding, generation, and translation.
Case Studies and Examples of Agentic AI in Healthcare RCM
While still in its early stages, agentic AI is already being used to address specific pain points in healthcare RCM:
- Eligibility Verification: AI agents can automate eligibility verification, reducing errors and ensuring accurate information for claims processing. For example, AI can search various data sets to identify patients’ active coverage much faster than a manual approach, accelerating access to care and increasing patients’ satisfaction with their health care experience.
- Claims Processing: AI agents can assist in reviewing claims, identifying discrepancies, and flagging potential issues for human review.
- Prior Authorization: AI agents can streamline prior authorization processes, reducing delays and improving efficiency. For example, an AI agent can sort through heaps of information quickly to verify each appointment and walk-in, ensuring that the services provided are eligible for reimbursement, and enabling them to inform the patients immediately if not, leading to improved patient satisfaction.
- Payment Posting: AI agents can automate payment posting, reducing manual errors and improving accuracy.
AI software can improve accuracy throughout the revenue cycle management process. AI greatly increases the accuracy of all patient and claims information. It also increases the accuracy of bills. This decreases the need for staff time to deal with follow-up questions and delays from the payer. The implementation of AI improves the efficiency of the RCM workflow process. Its increased accuracy allows for less follow-up work to fix errors. And it helps streamline many RCM operations.
Conclusion
Agentic AI has the potential to revolutionize healthcare revenue cycle management by automating tasks, improving efficiency, and reducing costs. By addressing key pain points such as claim denials, staffing shortages, and data management challenges, agentic AI can help healthcare providers optimize their financial processes and focus on delivering quality patient care. However, it’s crucial to address potential risks related to data privacy, bias, and transparency, and ensure compliance with relevant regulations. As agentic AI continues to evolve, it promises to transform healthcare RCM and improve the financial health of healthcare organizations.
The evolving healthcare landscape, with its increasing focus on value-based care and the adoption of new technologies, presents both challenges and opportunities for RCM companies. Agentic AI offers a powerful solution to navigate these complexities, enabling healthcare providers to improve efficiency, reduce costs, and enhance the patient experience. By embracing this technology and addressing potential risks, healthcare organizations can position themselves for success in the future of healthcare finance.