Healthcare providers today are under increasing pressure to optimize revenue while delivering exceptional patient care. One of the biggest challenges in this process is claim denial — a persistent issue that causes revenue loss, delays in reimbursements, and administrative burden. Fortunately, AI in healthcare claims is emerging as a transformative solution to this problem.
In this blog, we’ll explore how artificial intelligence is reducing claim denials, enhancing operational efficiency, and driving smarter decision-making in revenue cycle management.

✅ Understanding Healthcare Claim Denials
Before diving into the benefits of AI, it’s important to understand why claims are denied in the first place. Common reasons include:
- Incorrect or incomplete patient information
- Coding errors and mismatches
- Missing documentation
- Lack of medical necessity
- Payer-specific policy changes
Each denial not only delays payment but also consumes valuable resources in reprocessing and appeals.
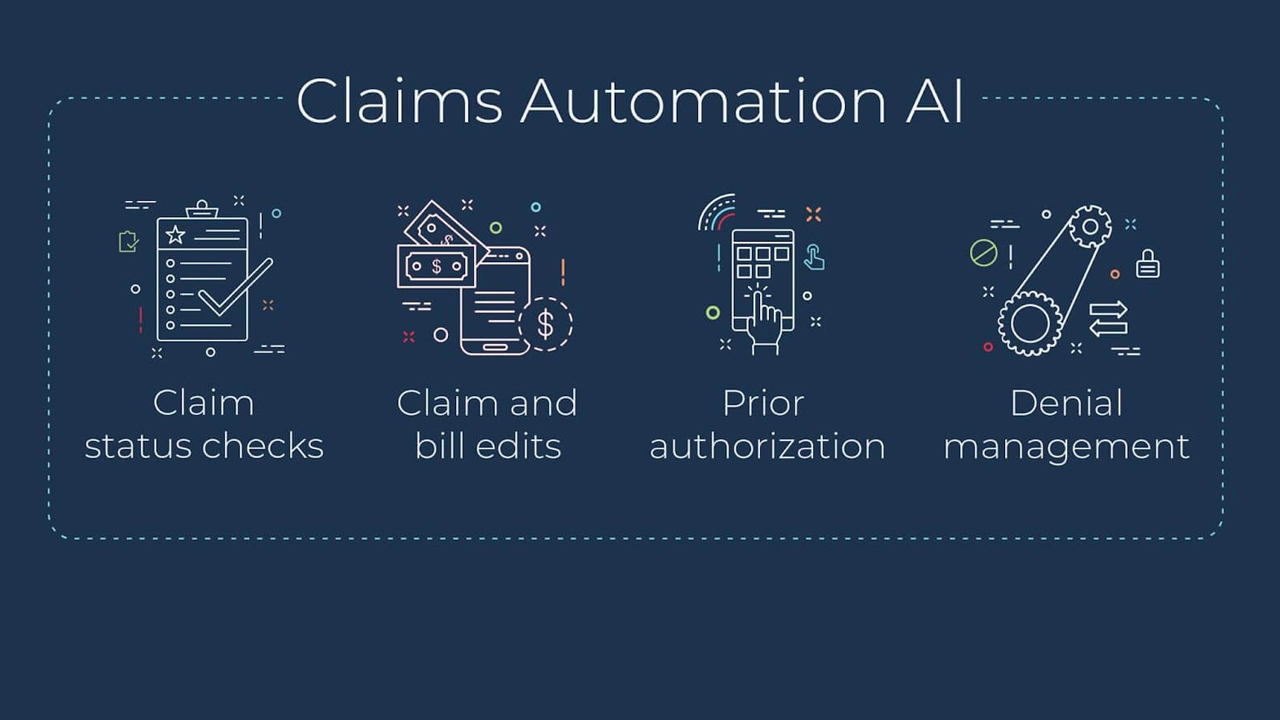
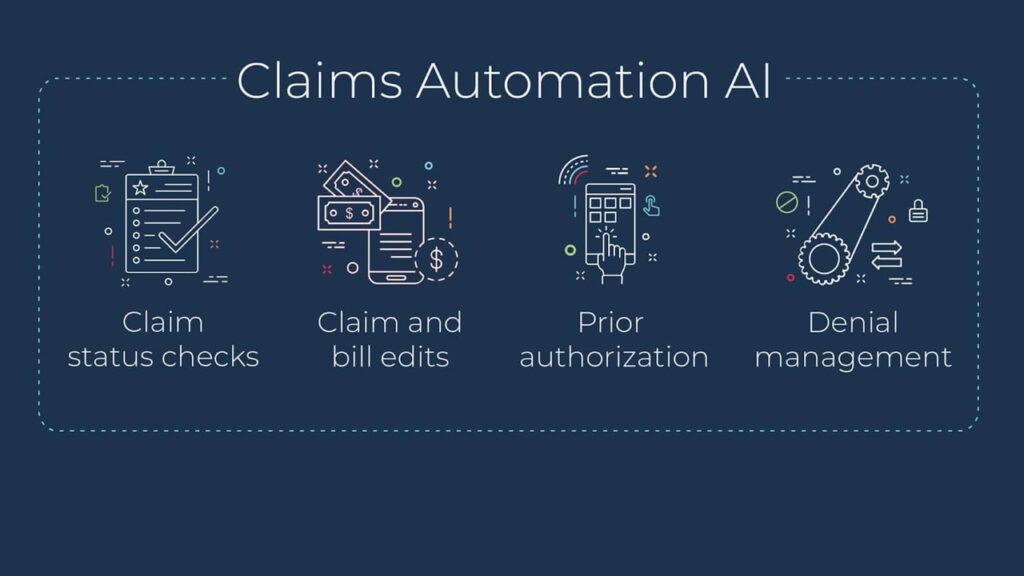
🚀 How AI Is Revolutionizing Claim Denial Management
Now, let’s take a closer look at how AI in healthcare claims can significantly reduce denial rates and streamline the entire billing process.
1. Predictive Analytics for Denial Prevention
To begin with, AI algorithms can analyze historical data and identify patterns that commonly lead to claim rejections. This enables healthcare providers to proactively correct issues before submission. For instance:
- Flagging incomplete forms
- Identifying high-risk claims
- Recommending coding corrections
Consequently, providers can reduce error rates and increase first-pass claim acceptance.
2. Automated Data Validation
Moreover, AI ensures accurate and consistent data entry by validating information in real time. This includes verifying:
- Patient demographics
- Insurance eligibility
- ICD/CPT coding accuracy
By automating this process, providers reduce manual errors and ensure cleaner claims submission.
3. Natural Language Processing (NLP) for Documentation
In addition, NLP-based tools extract relevant data from unstructured medical records and physician notes. This helps in:
- Automatically populating claims
- Attaching proper supporting documents
- Ensuring documentation aligns with payer policies
As a result, documentation-related denials are minimized significantly.
4. Real-Time Denial Management Dashboards
Furthermore, AI-powered platforms like Aiclaim offer real-time dashboards that allow revenue cycle teams to monitor denial trends. These dashboards provide:
- Instant visibility into rejection reasons
- Department-level performance insights
- Alerts for policy updates
Thus, teams can respond swiftly, improving turnaround times and reducing appeal costs.
🧠 Why Choose Aiclaim for AI-Driven Denial Management?
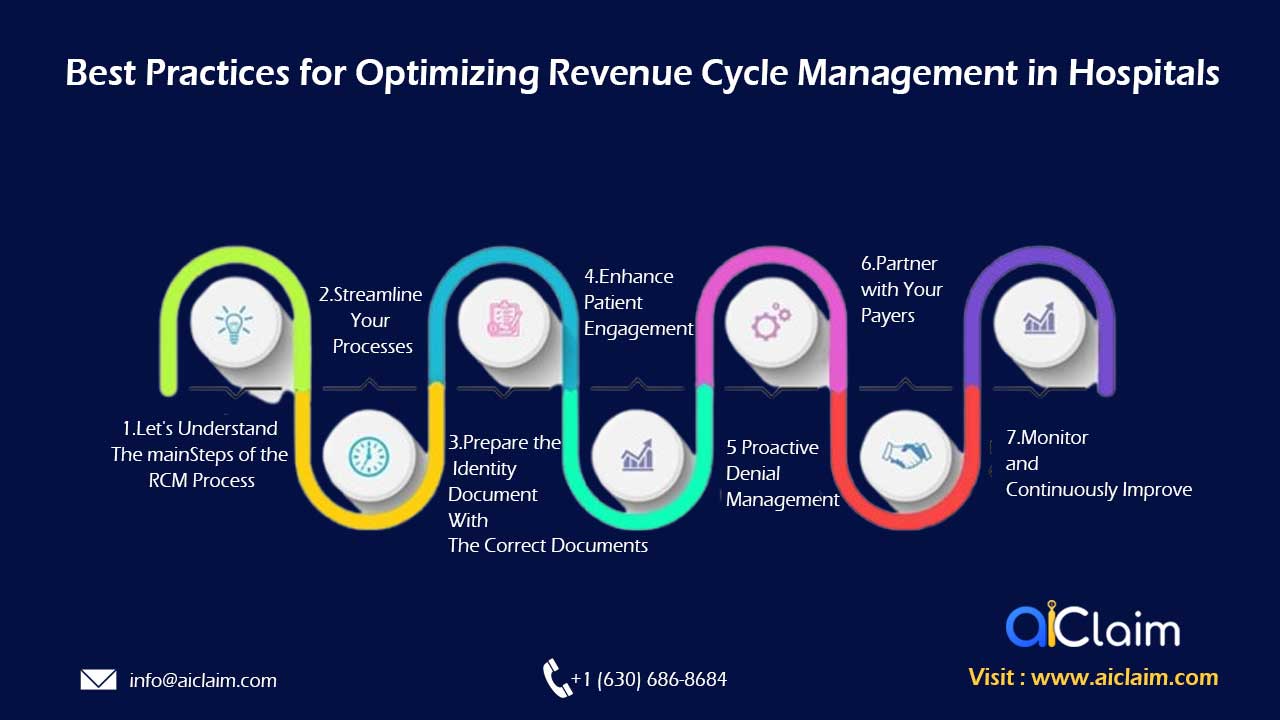
At Aiclaim, we specialize in advanced AI healthcare claims automation that helps providers reduce denials, recover revenue, and improve operational efficiency.
Here’s what sets us apart:
- End-to-end revenue cycle automation
- Real-time fraud detection and risk scoring
- Seamless EHR and payer integration
- Customized AI solutions tailored to your practice
Whether you’re a hospital, clinic, or a medical billing company, our tools empower your team to focus less on paperwork and more on patient care.
📈 SEO Benefits of AI in Healthcare Claims
From an SEO perspective, it’s important to highlight the long-term benefits of implementing AI:
- Increased claim acceptance rate
- Faster reimbursement cycles
- Higher patient satisfaction through smoother billing
- Better compliance with payer policies
Incorporating AI not only improves revenue but also strengthens your organization’s digital health infrastructure — a key ranking signal for healthcare businesses aiming for online visibility.
📝 Final Thoughts
In summary, AI in healthcare claims is not just a buzzword — it’s a powerful tool to reduce claim denials and optimize your revenue cycle. By leveraging predictive analytics, NLP, and automation, healthcare providers can achieve faster, more accurate reimbursements while staying compliant and efficient.
👉 If you’re ready to reduce denials and supercharge your RCM process, contact Aiclaim today to schedule a free consultation.