In the competitive world of healthcare revenue cycle management, insurance eligibility verification automation has emerged as a powerful game-changer. For decades, providers have relied on manual processes that often caused delays, errors, and unnecessary claim denials. Today, automation and AI are transforming this process, delivering faster reimbursements, fewer denials, and a smoother patient experience.
This blog explores how automation in insurance eligibility verification is revolutionizing healthcare, why it matters for providers, and how adopting AI-driven solutions ensures long-term success.
What is Insurance Eligibility Verification?
To begin with, insurance eligibility verification is the process of confirming whether a patient’s insurance plan covers the medical services they are about to receive. In other words, it serves as the first checkpoint in the revenue cycle to ensure that providers deliver services with financial accuracy and patients understand their responsibilities.
Specifically, the process ensures:
- First, active coverage validation so that providers know the patient’s insurance plan is current.
- Next, co-pay and deductible confirmation so that patients are aware of their upfront costs.
- Then, identification of pre-authorization requirements so that providers avoid delays in treatment approvals.
- Finally, detection of errors before claim submission so that costly rejections and denials can be prevented.
Traditionally, this process required staff to call insurance companies or log into multiple payer portals, and as a result, it consumed valuable time, increased administrative burden, and created opportunities for human error. Consequently, providers faced unnecessary delays, patients experienced billing confusion, and organizations struggled with revenue leakage.
However, with the rise of automation and AI, this process has transformed into a faster, more accurate, and highly efficient workflow. Therefore, healthcare providers can now eliminate bottlenecks, reduce costs, and enhance both financial performance and patient satisfaction.nto payer portals, which was time-consuming and error-prone. But with automation, verification becomes instant and accurate.
Why Automating Insurance Eligibility Verification Matters
The healthcare industry loses billions each year due to claim denials, many of which result from inaccurate eligibility checks. By shifting from manual methods to automation, providers can:
- Reduce claim rejections
- Improve cash flow
- Enhance patient satisfaction
- Save valuable staff time
In other words, automation ensures financial stability while improving the quality of patient care.
Key Benefits of Automated Insurance Eligibility Verification
1. Reduced Claim Denials
First and foremost, automated verification validates patient details in real time, and as a result, it minimizes the risk of errors that often lead to costly claim denials. Therefore, providers experience fewer rejections and enjoy a more consistent cash flow.
2. Improved Patient Transparency
In addition, patients are informed about their coverage, co-pays, and out-of-pocket costs upfront, and consequently, billing surprises are completely avoided. As a result, this transparency strengthens trust and improves the overall patient experience.
3. Faster Reimbursements
Moreover, automation reduces delays by submitting clean claims, and hence, it leads to quicker payer responses and faster revenue collection. In turn, healthcare organizations benefit from improved financial stability.
4. Higher Staff Productivity
Equally important, by eliminating repetitive manual tasks, healthcare staff can dedicate more time to patient engagement and financial counseling. Consequently, organizations not only improve staff satisfaction but also enhance patient support.
5. Compliance and Accuracy
Finally, automation ensures compliance with payer rules and significantly reduces the likelihood of regulatory violations. Thus, providers can maintain accuracy, avoid penalties, and safeguard their reputation.

How AI Enhances Eligibility Verification Automation
AI is not just about replacing manual tasks—it adds intelligence to the process. With AI-driven solutions, healthcare providers can:
- Predict claim outcomes based on past data
- Flag high-risk claims before submission
- Detect fraud and anomalies instantly
- Integrate seamlessly with EHR and billing systems
By combining automation with AI, providers not only streamline workflows but also optimize the entire revenue cycle management (RCM) process.
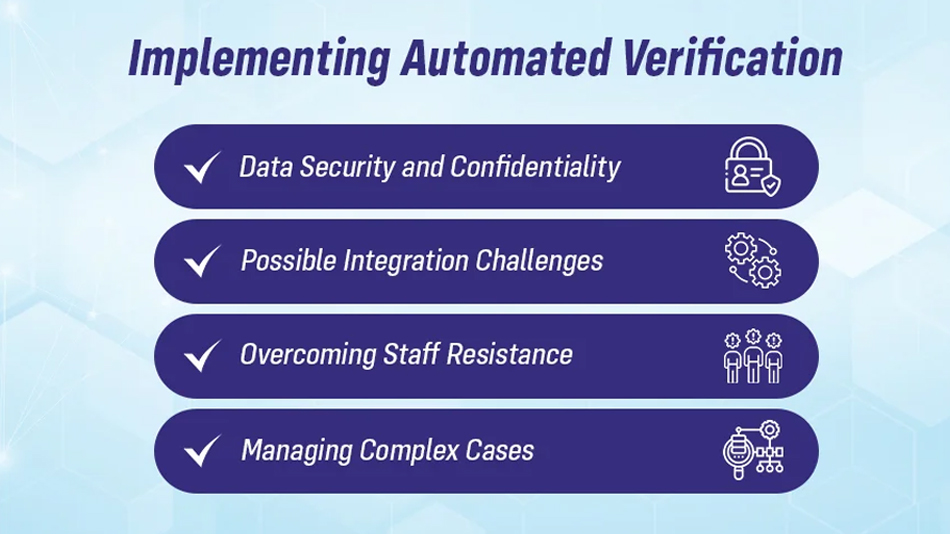
Why Choose Aiclaim for Insurance Eligibility Verification Automation?
At Aiclaim, we specialize in AI-powered healthcare automation that transforms revenue cycle management. Our eligibility verification solutions offer:
- Real-time coverage validation with payer integration
- Automated error detection to prevent claim denials
- Seamless integration with existing EHR/RCM systems
- HIPAA-compliant technology to ensure data security
Whether you are a small clinic or a large healthcare system, Aiclaim ensures faster reimbursements, reduced denials, and a better patient experience.
👉 Schedule your consultation today and see how automation can revolutionize your practice.
Final Thoughts
Automation in insurance eligibility verification is not just a trend—it is a necessity. By adopting AI-powered tools, healthcare providers can reduce denials, enhance patient satisfaction, and improve revenue cycle efficiency. In a future where every dollar counts, automation ensures accuracy, speed, and financial stability.
Don’t let outdated processes hold your organization back—embrace automation and unlock smarter healthcare operations.