The healthcare industry is evolving rapidly, and Artificial Intelligence (AI) is one of the biggest game-changers in claims processing. Lengthy approvals, endless paperwork, and costly human errors are becoming a thing of the past. AI is transforming how healthcare claims are managed by enabling faster approvals, improving accuracy, and reducing costs. As a result, insurers, healthcare providers, and patients all benefit from a more efficient system.
In this blog, we’ll take a closer look at how AI is revolutionizing healthcare claims processing. We’ll explore the key ways this technology is driving efficiency, reducing errors, and streamlining operations. More importantly, we’ll explore why organizations must embrace AI now to stay ahead of the curve. By adopting this technology, they can ensure a seamless and error-free future.

1. The Pain Points of Traditional Claims Processing
Healthcare claims processing has traditionally been a manual, time-consuming, and error-prone task. As a result, insurers and healthcare providers often struggle with inefficiencies that can lead to delays and increased costs. To better understand the impact of these challenges, let’s take a closer look at some of the key issues they face:
- Lengthy processing times – Manual verification and approvals often cause delays.
- Human errors & fraud risks – Mistakes in coding, duplicate claims, and fraudulent activities lead to losses.
- High administrative costs – Manual claims handling is expensive and inefficient.
- Compliance & regulatory issues – Changing healthcare laws and regulations make claims management complex.
These inefficiencies not only place a heavy burden on insurers and healthcare providers but also create unnecessary delays and frustration for patients who are eagerly awaiting reimbursement. Fortunately, this is where AI steps in to transform the process, bringing speed, accuracy, and efficiency to healthcare claims processing.
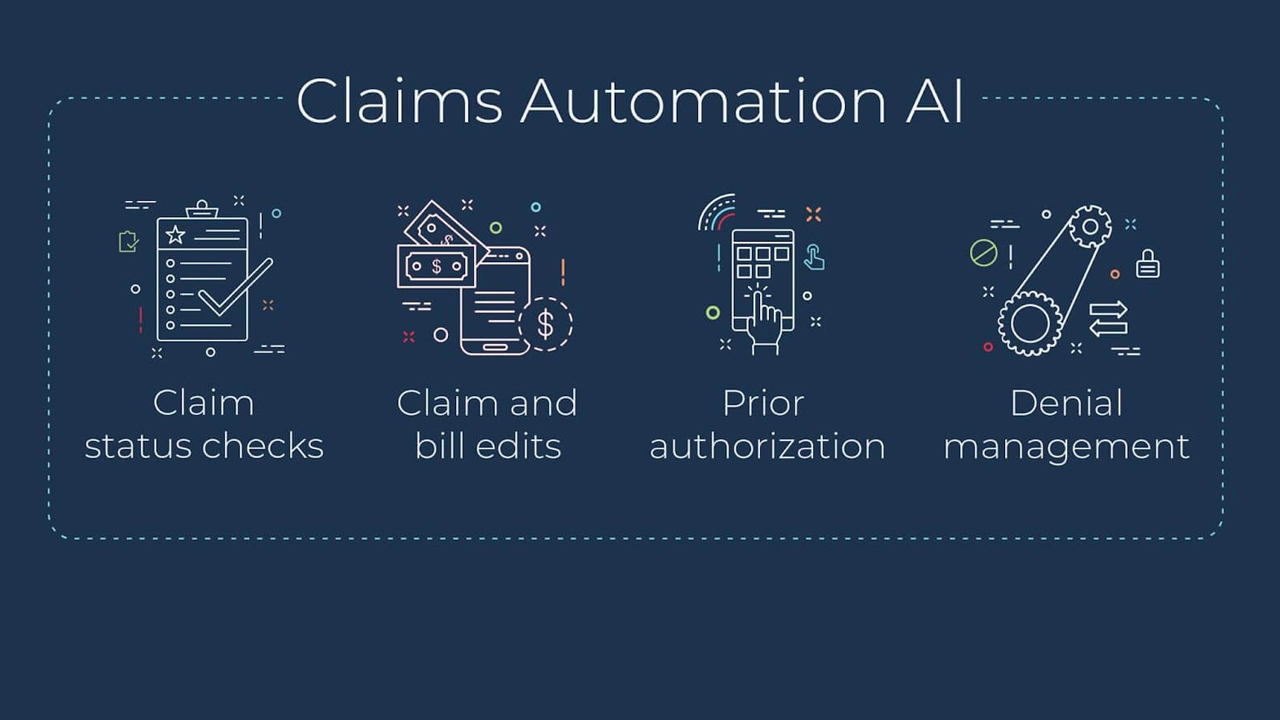
2. How AI is Transforming Healthcare Claims Processing
AI-driven automation is rapidly reshaping the landscape of healthcare claims processing by dramatically enhancing speed, accuracy, and efficiency. As this technology continues to evolve, its impact becomes even more evident in streamlining operations and reducing errors. To gain a deeper understanding of its transformative role, let’s explore the key ways AI is revolutionizing this process.
a) Intelligent Data Extraction & Processing
AI-powered Optical Character Recognition (OCR) and Natural Language Processing (NLP) are revolutionizing data extraction by seamlessly pulling information from handwritten documents, invoices, and medical reports with remarkable accuracy. As a result, AI significantly reduces the need for manual data entry, minimizing errors and accelerating processing times, which ultimately enhances overall efficiency.
b) Faster & Smarter Claims Validation
AI can efficiently cross-check claims against insurance policies, medical records, and regulatory guidelines to ensure they fully comply with all necessary standards before approval. In addition, Machine Learning (ML) algorithms can instantly verify the legitimacy of a claim, helping to detect discrepancies and prevent fraudulent activities. As a result, this not only streamlines the approval process but also eliminates unnecessary delays, ensuring a smoother experience for both insurers and patients.
c) Fraud Detection & Prevention
Healthcare fraud costs the industry billions of dollars each year, creating a significant financial burden for insurers and providers alike. However, AI is transforming fraud detection by identifying anomalies, spotting suspicious patterns, and flagging duplicate claims in real time. By proactively detecting fraudulent activities before they occur, AI helps insurance companies mitigate financial losses while ensuring that only legitimate claims are processed. This not only enhances security but also fosters a more transparent and trustworthy claims system.
d) Automated Decision-Making
With the power of predictive analytics, AI can intelligently assess a claim’s risk level by analyzing patterns and historical data. High-risk claims are immediately flagged for further review, ensuring thorough scrutiny, while low-risk, straightforward cases are automatically approved. As a result, this not only speeds up payouts but also optimizes resource allocation, allowing insurers to focus their efforts where they are needed most.
e) Enhanced Customer Experience
AI-powered chatbots and virtual assistants are transforming customer support by enabling patients to track their claims, receive real-time updates, and resolve queries instantly. By automating these interactions, AI significantly reduces the need for human intervention, allowing customer service teams to focus on more complex issues. As a result, this not only enhances operational efficiency but also improves overall customer satisfaction by providing quick and accurate responses.
3. The Real Benefits of AI in Healthcare Claims Processing
The adoption of AI-powered claims processing is leading to major advantages for the entire healthcare ecosystem:
Faster Claim Approvals – By automating processes, AI reduces claim processing time from weeks to mere hours or minutes.
Increased Accuracy – With advanced algorithms, AI eliminates human errors, ensuring claims are processed correctly.
Cost Savings – Automation significantly reduces operational expenses by minimizing manual work and preventing fraud-related losses.
Improved Compliance – By cross-checking claims against regulatory policies, AI helps organizations avoid legal complications.
Better Fraud Detection – Suspicious patterns and anomalies are identified early, allowing insurers to prevent fraudulent claims.
Enhanced Customer Experience – Patients and providers benefit from quicker resolutions, fewer disputes, and a more seamless process.
4. Future of AI in Healthcare Claims Processing
The AI revolution in healthcare claims processing is just beginning! Here’s what to expect in the future:
AI-driven blockchain integration enhances security by ensuring transactions remain tamper-proof and transparent.
Predictive analytics helps forecast trends, allowing insurers to optimize claims handling strategies proactively.
Personalized AI solutions adapt to the unique needs of insurers and healthcare providers, improving efficiency.
Greater interoperability between AI systems and electronic health records (EHRs) enables seamless data sharing and better coordination.
As AI technology continues to advance, claims processing will become even more efficient, cost-effective, and reliable. Healthcare organizations that adopt AI-driven solutions will stay ahead of the curve, ensuring faster approvals, fewer errors, and bigger savings!
Final Thoughts
AI is not just the future—it’s the present of healthcare claims processing. By automating tedious tasks, reducing errors, and enhancing fraud detection, AI-powered solutions are revolutionizing how insurers and healthcare providers handle claims.
If you’re in the healthcare or insurance industry, now is the time to leverage AI to improve efficiency, reduce costs, and enhance customer satisfaction.
Want to explore AI solutions for claims processing? Let’s talk! 🚀